Introduction
Regional anesthesia plays a pivotal role in modern surgical
procedures, offering targeted pain relief and potentially
improving postoperative outcomes. Unlike general anesthesia,
which induces a state of total unconsciousness, regional
anesthesia numbs a specific area of the body, allowing
patients to remain awake or sedated without affecting their
overall consciousness. This approach can lead to faster
recovery times, reduced hospital stays, and, in many cases,
fewer side effects.
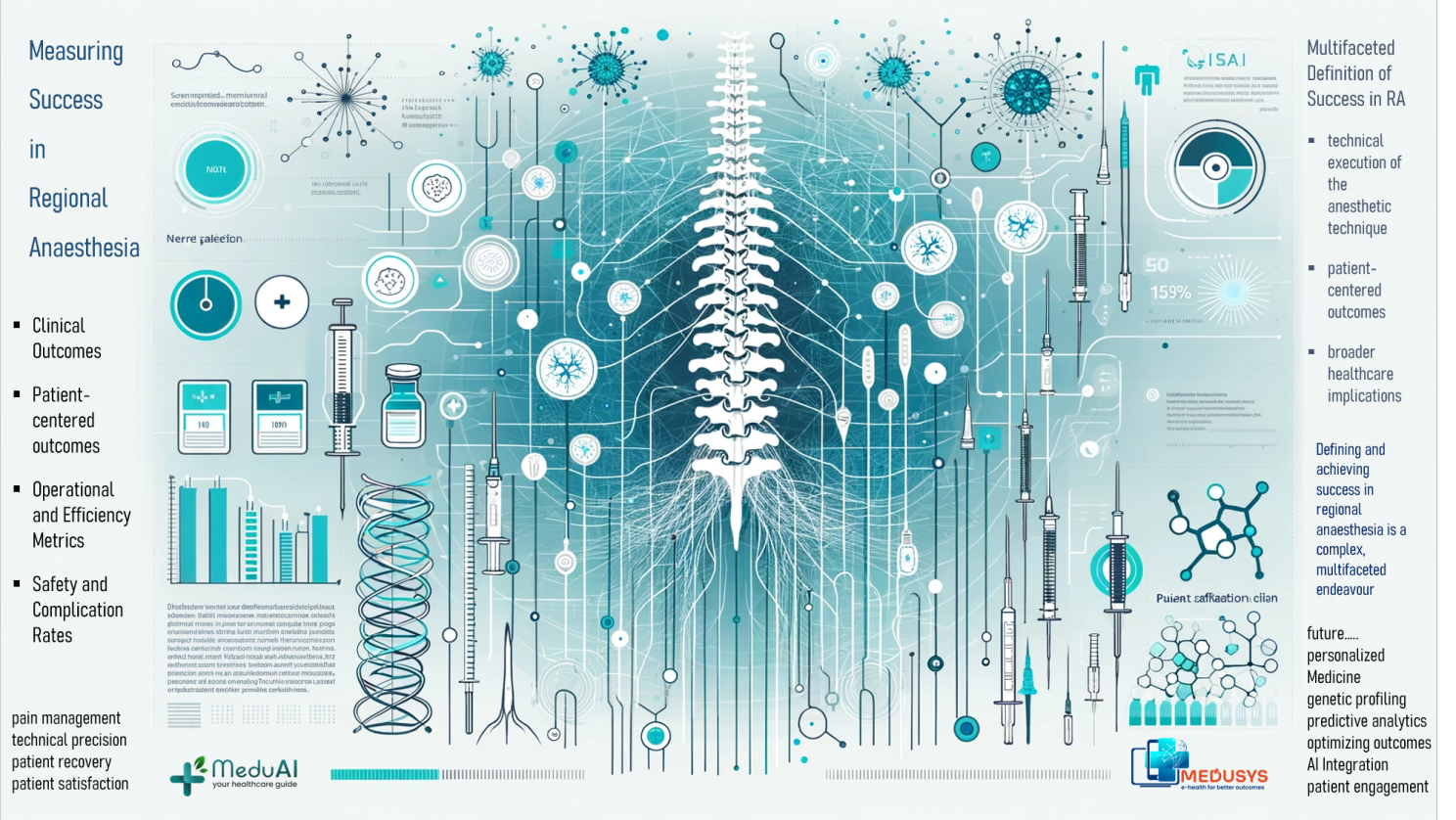
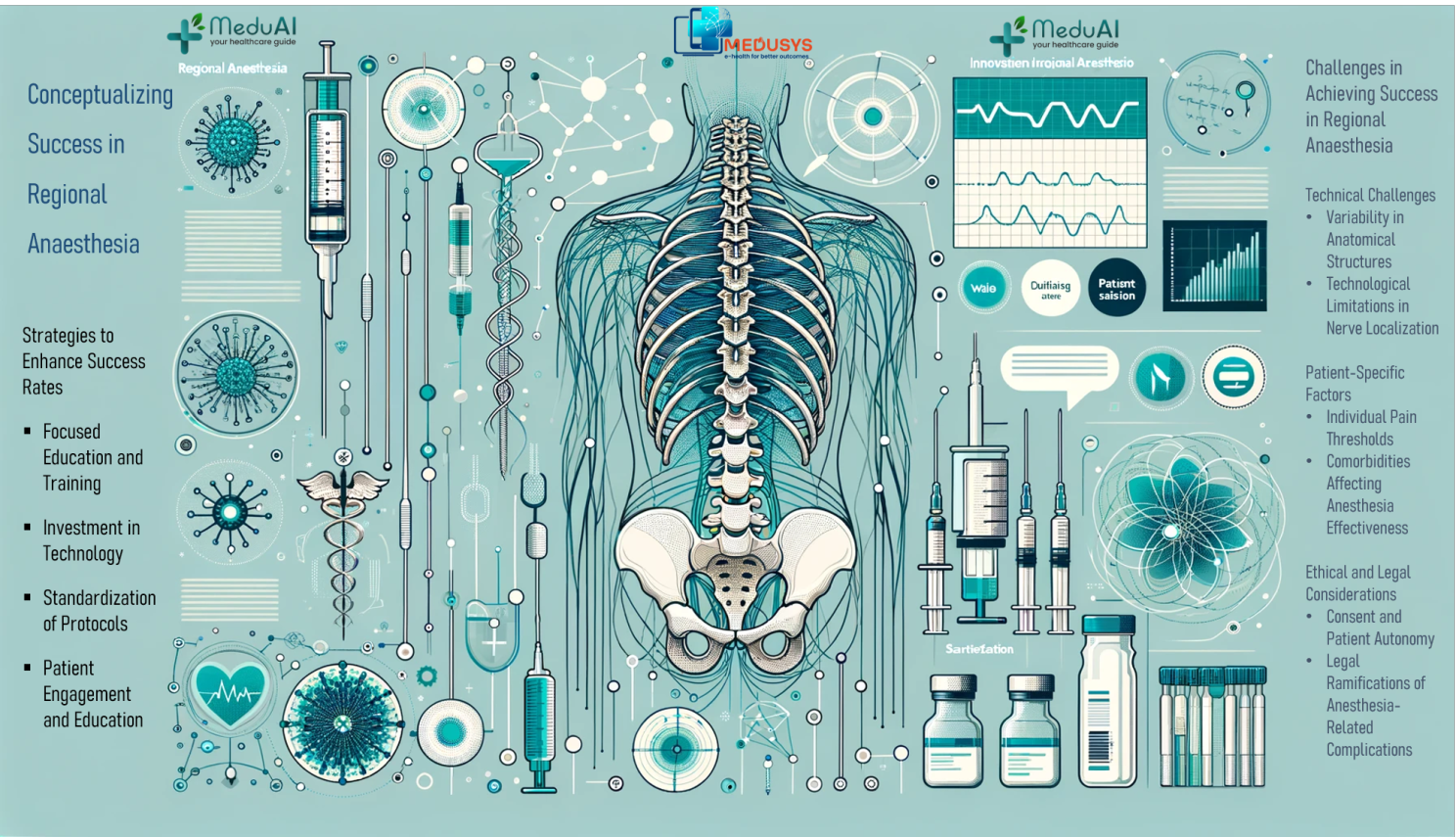
Defining success in regional anesthesia is multifaceted,
encompassing not only the
(1) technical execution of the anesthetic technique but also
(2) patient-centered outcomes and (3) broader healthcare
implications.
As such, success criteria can range from the immediate
effectiveness in pain management and the precision of nerve
blockades to long-term patient satisfaction and economic
impacts on healthcare systems. In the following sections, we
will delve into these various dimensions, examining how each
contributes to a holistic understanding of success in regional
anesthesia. This article aims to provide healthcare
professionals, patients, and policymakers with a comprehensive
framework for evaluating and enhancing the practice of
regional anesthesia in clinical settings.
In the following sections, we will delve into these various
dimensions, examining how each contributes to a holistic
understanding of success in regional anesthesia. This article
aims to provide healthcare professionals, patients, and
policymakers with a comprehensive framework for evaluating and
enhancing the practice of regional anesthesia in clinical
settings.
.png)